Investigating the learning value of early clinical exposure among undergraduate medical students in Dubai: a convergent mixed methods study | BMC Medical Education

Out of those 68 students, 54 responded (i.e., response rate = 79.41%).
Quantitative
The reliability score of Cronbach’s Alpha for the ‘ECE Familiarization’ tool was 94.90%. The percentage of the total extent of agreement of ‘ECE Familiarization’ score was 79.60%, as per Table 1. According to the PCA (Kaiser–Meyer–Olkin Measure of Sampling Adequacy), 82% of the variance can be explained by the instrument (p < 0.001). Along the same lines, the Bivariate Spearman Correlations showed how the changes in the ‘ECE Familiarization’ score can be explained by changes in all fifteen components. Moreover, all components were associated with each other (p < 0.05).
The reliability score of Cronbach’s Alpha for the ‘Visibility of Values’ tool was 92.60%. The percentage of the total extent of agreement of ‘Visibility of Values’ score was 86.43%, as per Table 1. According to the PCA (Kaiser–Meyer–Olkin Measure of Sampling Adequacy), 88.40% of the variance can be explained by the instrument (p < 0.001). Along the same lines, the Bivariate Spearman Correlations showed how the changes in the ‘Visibility of Values’ score can be explained by changes in all six components. Moreover, all components were associated with each other (p < 0.001).
As for the ‘extent of active engagement and self-directed learning’, the percentage of the total average was 68%, as per Table 1. The ‘extent of active engagement and self-directed learning’, with a mean of 6.80(2.42), seemed to be significantly associated with both the ‘ECE Familiarization’ and the ‘Visibility of Values’ scores (P < 0.05). The ‘extent of active engagement and self-directed learning’ also seemed to be significantly associated with the following components of the two tools: Learning in the clinical environment, Health system functioning (e.g., settings of care, patient journey, and integrated care), Professional identity of healthcare providers, Importance of certain competencies (i.e., knowledge, skills, and attitudes) for clinical care among healthcare providers, Pressures on healthcare providers, Patient perspective of health and illness, and Hygiene and infection control practices, and Integrity and Empathy (P < 0.05).
In relation to ‘ECE Familiarization’ score, it seemed to be associated with ‘Visibility of Values’ score and all its components (P < 0.05). Besides its significant association with ‘Visibility of Values’ score, ‘ECE Familiarization’ turned out to also be significantly associated with all the ‘Visibility of Values’ score components (P < 0.05). As for ‘Visibility of Values’ score, besides its significant association with ‘ECE Familiarization’ score, it was significantly associated with all its components (P < 0.05), except for: Documentation (i.e., Electronic Medical Record keeping) (P = 0.21).
Qualitative
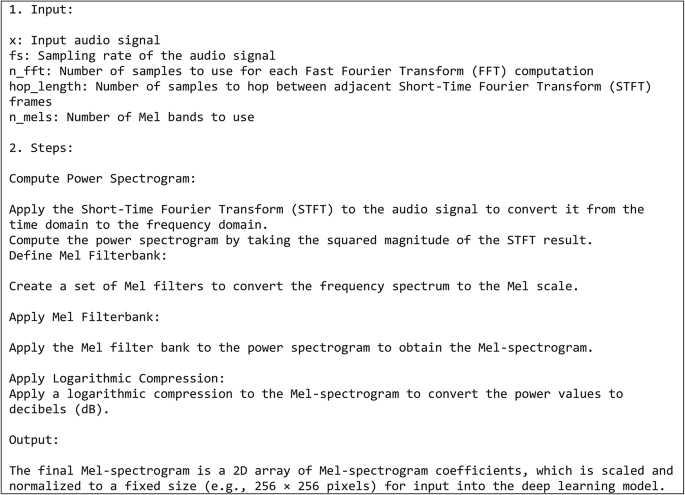
The qualitative analysis led, as per this study’s conceptual model: ‘Early Clinical Exposure Added Value’ (Fig. 5), to five interconnected themes, namely: Orientation, Learning, Self-efficacy, Professional identity, and Foresight. Within Orientation, two categories were identified: Realism and Familiarization. Within the second theme: Learning, the following four categories were identified: Self-regulation, Clinical correlations, Value of doing things right, and Challenges. Within the third theme: Self-efficacy, the following two categories were identified: Motivation and Confidence. As for the fourth theme: Professional identity, it encapsulated: Purpose and Professionalism. Lastly, within the fifth theme: Foresight, the following three categories were recognized: Impression, Expectations, and Progression.
Early Clinical Exposure Added Value
The tally of the count of participants that brought up matters relevant to each of the categories showed the distribution, outlined in Table 2.
Orientation
This theme included any text fragment that reflects how the learning experience made the students more acquainted with learning and practicing in the clinical environment.
Realism
This category encapsulated all the text fragments that show the students’ perception of how this learning experience, which goes well beyond the classroom setting, embedded the students in the authentic context of learning.
15: ‘…realistic depiction of what happens usually in a hospital setting…’
40: ‘…it helped us learn things that cannot be taught in class…’
According to the students, the experience offered them a ‘reality-check’. They frequently described it as ‘novel’.
36: ‘…interactions with real patients and observations of real procedures…’
A few students considered the experience a pleasant change of setting.
22: ‘…also it was fun to go to a hospital, it was a ‘change of air’ to have in the middle of the academic semester…’
34: ‘…a positive change in the environment coupled with a fun, meaningful experience…’
Among the characteristics that stood out to the students the most in the clinical environment was the shared decision making between the healthcare providers and the patients. They seemed to recognize instances where healthcare providers strove to maximize their engagement with patients.
10: ‘…understand treatment options differ; it becomes more about making decisions with the patient…’
It seemed that the ECE brought to the attention of the students the sophistication of the practice of medicine. Several students highlighted the uncertainty and relativity integral to this practice.
28: ‘…applying it in a real-life scenario is not always as simple and straightforward…’
48: ‘…one thing I learnt is that there are no absolutes, white or black, ‘definite’ areas in medicine. There will be instances where one thing accommodates for another or compensates for it, and that is normal. This again confirms the widely circulated phrase in the field of medicine: ‘one size does not fit all’…’
Familiarization
This category included all the comments that show an increase in awareness about the characteristics of learning in the clinical environment. Students seemed to recognize distinct attributes and also reflected on how those features are interconnected which is essential for the functioning of the health system, emphasizing that ‘the whole is more than the sum of its parts’.
8: ‘…introducing students to other clinical settings like triage rooms or emergency departments where they will be more likely to interact with patients and view integrated healthcare in action….’
44: ‘… seeing the operations of different elements of the healthcare system and how these different elements interact…’
Among the attributes that they indicated were ones related directly to the placement site in which they were present for the learning experience. Many of the students reflected upon the logistics of commuting to and from the placement sites and their preferences in that regard.
8: ‘…familiarizing ourselves with the commute…’
The students also highlighted attributes related to the people within the placements.
1: ‘…interacting with patients and learning through observing physicians…
The ECE seemed to have increased their awareness of the patient perspective, and the healthcare providers’ roles and responsibilities.
5: ‘…I have a greater understanding of the patients’ perspective as I progress through my medical learning…’
They noticed the (often competing) pressures on the healthcare providers. The learning opportunity also shed light on several aspects of the patient-healthcare provider interactions, which include communication, privacy, and confidentiality.
9: ‘…exposes me to how health professionals interact with the patient…’
The means by which the healthcare providers conducted themselves was also apparent to the students, where the students either knowingly or otherwise pointed out embodiment of one or more of the institutional values.
15: ‘…gaining knowledge on how to act in a hospital setting (e.g., interaction between colleagues and with patients)…’
37: ‘…it was a good introduction to the clinical setting; we observed different departments and saw how they worked together to realize the value of patient first…’
It seemed that the ECE enabled the students to attribute a meaning to the term: ‘professional identity’, which they have been conceptually learning about for some time. They also saw firsthand the interprofessional teamwork that takes place in the clinical setting.
37: ‘…I enjoyed our discussion with a physician about the roles of different people that work together to rescue a patient in an emergency situation…’
48: ‘…appreciating how different things usually run in a clinical setting (e.g., patient-doctor interaction and interprofessional teamwork)…’
The ECE also brought to the attention of the students the workflow within the clinical setting and factors that affect it.
43: ‘…exposing us to …how health care is provided to the patients from the moment they enter the clinic until they leave…’
Several students also mentioned either directly or indirectly policies and procedures, including those related to documentation, and hand hygiene and infection control practices.
21: ‘…getting familiar with the system and knowing what is expected of me (e.g., how to handle situations and maintain patient confidentiality)…’
37: ‘…I observed a nurse communicate and take vitals from a patient. She then talked me through the documentation process and discussed with me how this information would reach the physician…’
Learning
This theme included the students’ reflections on the personal and/or collective growth that they experienced through observing in the clinical setting as part of the ECE.
Self-Regulation
This category highlighted the students understanding of self-directed learning.
42: ‘…like one of the doctors mentioned in the foundation of clinical medicine course: ‘you have to go out and look for medicine, it will not come to you’. I made sure to take full advantage of this opportunity…’
Being proactive through asking and answering questions, and through attentively listening were identified as key ways by which the students considered themselves to have engaged in their own learning. The students frequently highlighted incidences where they interacted with the healthcare providers, who served as educators in the authentic context of learning.
14: ‘…I was answering questions asked by the doctor and asking questions when I had ones…’
20: ‘…I tried my best to engage with the nurses and doctors, and to listen to the patients as much as I can.
Some students reflected upon how they prepared for the respective learning opportunity.
15: ‘…prior to entering the center, I tried utilising various resources to understand how dialysis works and review previous content relevant to kidneys and their physiology…’
Other students managed to get involved in the provision of care and not solely observe it.
24: ‘…I put in effort by asking questions and engaging with the staff. I also helped with taking history of patients, and taking the initiative, at one point, to bridge the language barrier between the provider and a patient…’
For students, taking an active role in their own learning had two prerequisites. Firstly, they seemed to recognize that they need to ‘step out of their comfort zone’, and to demonstrate proactivity, as well as (a degree of) adaptability.
1: ‘…I have actively engaged to maximize my learning in the clinical setting…’
15: ‘… see how knowledge can be applied in the clinical setting… find gaps in our current knowledge base, and what is needed to bridge these gaps to reach the expected performance…’
Some students even mentioned the value of developing plans and exercising particular learning strategies. Relevant to those examples, the students seemed to believe that the opportunity to maximize their learning lays within their control.
18: ‘…seeking out opportunities and leveraging self-directed learning strategies that maximize the educational value of the exposure…’
Several students appeared to be fairly assessing the extent of proactiveness that they deployed, where they reflected on whether they could have ‘done a better job’.
12: ‘…I think I could have better communicated and found a way to be more helpful in the setting and tried to ask more questions…’
23: ‘…I could have asked more questions…’
Those students seemed to assign value to their curiosity and hold themselves accountable to their own learning, where some of them highlighted their nervousness as a factor that held them back from learning during the placement.
20: ‘…I was curious to learn about the patient cases, and to figure-out whether, or not, I have studied them in the past year and a half…’
44: ‘…I could have engaged more actively with the consultation… I was asked whether, or not, I wanted to take history, but truthfully, I was feeling nervous, thought I would be more comfortable to stick to just observing the consultation…’
Secondly, the students seemed to believe that the opportunity for engagement must be present; proactivity alone is not enough. They highlight that the required opportunity for engagement is determined by factors outside their control, including the attitudes of and dynamics with healthcare providers, as well as the activities within the clinic, such as patient flow.
20: ‘…some nurses or doctors were not sufficiently engaging…’
47: ‘…I tried my best to engage with the program, but I did not get the same energy back…’
This is where several students made suggestions of how the ECE can become more engaging.
43: ‘…a good way to improve the early clinical exposure would be to provide some more guidance about how to approach it and what to expect so that we do not get overwhelmed as it is the first time we get exposed to such an experience…’
Clinical correlations
This category related to the growing understanding, among students, of the relevance of the lessons taught in the classroom.
6: ‘…seeing how what we have learned in class applies in the clinical setting…’
17: ‘…connected what we are learning on-campus to real life…’
Many of the students’ comments were about how their observations in the clinical setting related to the curricular knowledge they have been acquiring. They saw how the theoretical knowledge is applied in the clinical setting.
44: ‘…to see how the theories and frameworks we learn in class can be translated into practice and applied in a clinical setting…’
45: ‘…I get to connect what I learn from books and lectures to real-life interactions with patients…’
At several instances, the students seemed to be comparing and contrasting learning environments, describing the placements as ‘richer’ relative to all that they experience on campus.
37: ‘…we are able to learn skills that are more difficult to grasp in a typical classroom setting; for example, how the healthcare team works together is best learned through observation of the team in action…’
42: ‘…much richer compared to theoretical knowledge learned in lectures…’
They considered the ECE to offer them opportunities to identify gaps in their knowledge and strive to bridge them.
12: ‘…A lot of things seem less sophisticated when written on/read from books, but seeing the same topics applied in hospitals and clinics shows a new perspective that can help a student feel more comfortable in their future practice…’
54: ‘…work on improving some of the skills that we learnt in the foundations of clinical medicine course …’
The students identified competencies that they may have acquired, some of which were intended, including soft skills, such as: communication, professionalism, and empathy.
13: ‘…contributes to improving communication skills… it is a form of professional development…’
18: ‘…it enhances communication skills, empathy, and the understanding of patient care…’
The students also highlighted other competencies which were not intended learning outcomes of the ECE, such as: pathological basis of disease.
7: ‘…in the placement at the dialysis center, we heard lung crackles and examined fistulas, and talked to multiple patients. The doctor gave us an explanation of chronic kidney diseases; it was very informative…’
10: ‘…helped me link the theory learnt to clinical presentations of patients…’
Value of doing things right
This category related to text fragments that show the importance that the students attributed to certain competencies that they observed during the ECE, and how those competencies, according to the students, make the patients feel valued.
12: ‘…I now know what practices contribute to providing better services to patients…’
27: ‘…how important it is to understand and actually care for the patients…’
The students reflected upon how those competencies affect the patients’ experience of care and ultimately its outcomes.
12: ‘…I have also seen practices that might have made patients feel less welcome and less important, for which I will try to avoid doing during my service and practice as a future physician…’
32: ‘…the influence of doctor-patient dynamic on the delivery and outcomes of patient care…’
The students brought-up many skills with particular emphasis on interpersonal ones.
41: ‘…brings forth the importance of respect and autonomy…’
45: ‘…it teaches me crucial qualities that include empathy and teamwork…’
The importance of effective teamwork was (actually) repetitively alluded to.
32: ‘…allows medical students to understand the impact of effective teamwork in the clinical environment…’
Challenges
This category related to the difficulties in learning that the students experienced while participating in the ECE intervention.
12: ‘…there were several barriers to interacting with doctors. We were able to shadow nurses yet given that they were so focused on their work, they rarely engaged with us or supported us in learning about their systems and processes…’
Some of these difficulties were due to characteristics of the respective learning intervention. In other words, the ECE was designed in a particular way, with specific learning outcomes, which define and in turn limit its overall scope. For example, the students needed to commute to the placements and were meant to be in the authentic context of learning for a limited period of time.
2: ‘…we were there for a short time, and could not see and in turn learn much…’
6: ‘…during our visit, we barely saw any patients. I only saw the intake of one patient by a nurse…’
Some students offered suggestions for improving the logistics of the learning intervention. For example, providing the students with transportation was brought-up several times.
54: ‘…I suggest that transportation should be provided to the placements’ site…’
For some students, establishing the link between what they had observed as part of the ECE and their coursework was not a straightforward exercise.
4: ‘…it had not that much to do with the actual courses we are taking…’
The disparities in the learning experiences were also repetitively alluded to by the students as challenges to learning as part of the ECE.
30: ‘…from speaking to my colleagues, I can tell that my experience was far better than most of them, so not everyone was able to get the same insight into health care…’
Ultimately, the ECE is a direct reflection of the clinical environment, in terms of the activities that take place including but not limited to those relating to the patient flow. Variations in what the students get exposed to are inevitable..
44: ‘…experiences varied depending on the centers they visited and the time of the visit, so some might not have had the same opportunities as others…’
50: ‘…the disparity between my two visits underscores the variability in clinical exposures, emphasizing the importance of consistent, active engagement from our side for a comprehensive learning experience in medical education…’
Self-efficacy
This theme related to the students’ reflections of how the ECE increased their self-efficacy and in turn resilience in learning and in practicing medicine.
Motivation
This category encapsulated how the ECE contributed to increasing the students’ enthusiasm to engage more in their own learning as they are training to become future doctors.
22: ‘…it motivates us to keep-up with our studies…’
45: ‘…it helps boost motivation towards my studies as it shows me a glimpse of my future…’
ConfidenceS
This category highlighted the text segments that related to the students’ increased capacity of tolerating uncertainty.
10: ‘…it increases confidence in learning among students…’
31: ‘…feeling more confident and comfortable in a clinical setting…growing confidence upon better understanding patient needs and witnessing teamwork…’
The ECE was frequently described, in a way or another, as an ‘enabling experience’.
53: ‘…exposing us to several rounds of clinical history taking and consultation, which is quite enabling…’
Professional identity
This theme included all the ways by which the students describe the development of themselves in relation to the profession of medicine.
Purpose
This category related to how the students felt that the experience is reinforcing their ‘raison d’être’.
8: ‘…allowing us to meet patients face-to-face serves as a reminder of who we are studying all of this for so as not to become apathetic to disease and its impact…’
20: ‘…to understand what we are studying to become…’
Several students expressed that the ECE highlighted to them the significance of what they are after: their sense of purpose.
27: ‘…it shows me what my job will be as a healthcare practitioner all about…’
33: ‘…understanding the role of the doctor in the community…’
Several students emphasized that serving others appeared to be at the core of the profession of medicine. They appeared to have come to this realisation through observing that healthcare providers are constantly striving to ease patients’ pain.
16: ‘…it helped me know that this profession requires that I always ‘give it my all’, regardless of how many patients a doctor sees. Every patient deserves to be listened to, respected, and helped…’
The students saw firsthand how physicians realize their purpose.
42: ‘…realizing that everything we learn in lectures can contribute to one day treating a patient and easing their pain…’
Professionalism
This category related to the students’ reflections on the competencies and values that are shared among healthcare providers, in general, and physicians, in particular.
24: ‘…development of professional values and patient-centered care…’
54: ‘…… it helps in developing our professional identities by observing doctors interacting with their patients…’
The students emphasized the behaviours and attitudes that they consider ‘professional’.
15: ‘…it helps us envision the core values we need to be a successful doctor…’
44: ‘…learning to internalize and adopt the proper attitudes; observing effective communication skills early on will help us become more efficient, empathetic doctors moving forward…’
They also highlighted how the ECE enabled them to connect with and get to know role models who inspired them.
25: ‘…learning professional behaviour…very interesting, knowledgeable doctors…’
Foresight
The last theme included the students’ reflections of how the ECE raised their visibility in terms of their educational and professional trajectory.
Impression
This category showed that the ECE gave the students insight into their future careers, where they became better positioned in exploring and in turn identifying their interests.
16: ‘…it helps us see what we are interested in…’
The students highlighted how the ECE prepared them for upcoming stages.
34: ‘…giving us a glimpse at clinical life…’
38: ‘…getting a feel of interacting with real patients… develop insight into clinical practice…’
This learning experience shed light on the day-to-day work of doctors with particular emphasis on interacting with patients and striving to help others.
6: ‘…it gives us an idea of what our workdays will be like in the future…’
52: ‘…it gives me an idea of how I could help people if I were in the doctor’s place…’
Expectations
This category revolved around how the ECE enabled the students to manage their expectations.
29: ‘…helps us answer some of our future questions with regards to the specialities we would like to pursue…’
48: ‘…it orients us in terms of managing our expectations and setting professional standards…’
They associated the ECE experience with developing their personal and professional resilience.
7: ‘…the earlier we get used to clinical environment, the better we are at handling stress later during rotations and residency…’
8: ‘…sensitizing us to the general conditions of clinical care settings to minimize surprises when beginning our clinical learning in Year 4…’
Progression
This category related to descriptions of the progressive nature of the students’ learning and career trajectories.
11: ‘…a new introduction in my medical journey…’
47: ‘…ECE is a good step forward…’
The reflections of the students showed that they are clearly differentiating between early clinical exposure and learning in clinical environment.
13: ‘…learning in the clinical environment means hands-on learning in a real healthcare setting as opposed to a classroom or theoretical environment…’
32: ‘…being exposed to the clinical environment early on to understand the requirements needed for later years as medical students as well as the dynamic needed for our future careers…’
The students’ reflected on different upcoming steps.
10: ‘…make us better prepared to start clinical rotations in Year 4…’
44: ‘…throughout the subsequent years, we can build upon and refine this foundation…’
In terms of the value of the ECE, the students also differentiated between the short-term value which, according to them, related to preparing for learning in the clinical environment, and the long-term value which, to them, was about becoming better future physicians.
18: ‘…early clinical exposure provides immediate benefits like increased engagement in learning and observing for the betterment of communication skills
22: ‘…longer term effect of this early exposure is that it helps us to become better physicians…’
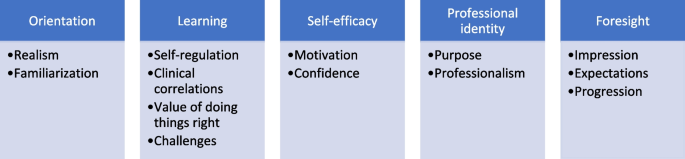
Integration
Integrating the output of the quantitative analyses with that of the thematic analysis revealed a holistic understanding of the learners’ perception of the subject matter, illustrated in the study’s side-by-side joint display (Fig. 6). The integration of findings (i.e., primary inferences) enabled the development of a thorough understanding of the learners’ experience with ECE. As such, integration led to six meta-inferences: Embeddedness in context of learning, System perspective, Patient-centricity, Theory–practice link, Resilience, and Proactiveness. There appeared to be a mutually reinforcing relationship—a virtuous cycle—between the learners and the learning integral to ECE across all six domains of the meta-inferences. In other words, the more committed the learners were to engage with any of the six domains, the more ECE advanced their progress in that direction.
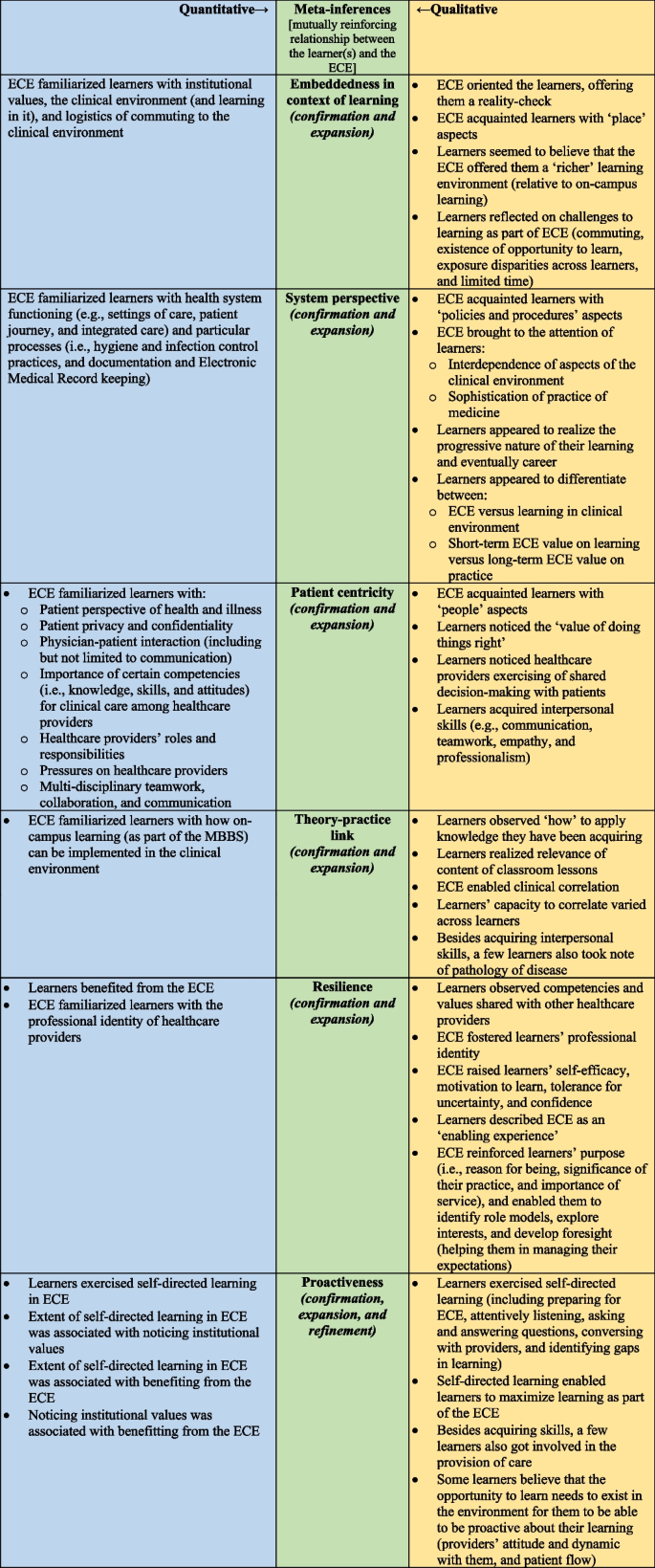
Output of the iterative joint display analysis process, resulting in six meta-inferences: Embeddedness in context of learning, System perspective, Patient centricity, Theory–practice link, Resilience, and Proactiveness. The secondary color Green emerged by mixing the primary color Blue with the primary color Yellow (which constitutes an analogy of the lateral and critical thinking that took place to generate the meta-inferences from the integration of two sets of primary inferences). For the first five meta-inferences, integrating the quantitative with the qualitative inferences led to both: confirmation and expansion in the overall viewpoint. As for the last meta-inference, namely: Proactiveness, the integration led to: confirmation, expansion, and refinement of the overall viewpoint
The quantitative analyses indicated that the ECE helped learners become familiar with the clinical environment and the learning that occurs within it. Similarly, the qualitative analysis demonstrated that the ECE oriented learners to the context, providing them with a reality check. Additionally, the qualitative analysis revealed that students regarded learning in the clinical environment as ‘richer’ compared to the on-campus setting. The challenges associated with learning in the clinical environment were also clearly articulated by students in the narrative data. Thus, for the’Embeddedness in context of learning’meta-inference, the integration enabled both confirmation and expansion of the overall perspective.
For ‘System perspective’ meta-inference, the ECE helped learners understand how health systems function and the key processes involved. In line with this, the qualitative data analysis demonstrated that the ECE introduced learners to policies and procedures, highlighting how ‘the whole is greater than the sum of its parts’ in health system functioning. Furthermore, the qualitative analysis revealed the students’ awareness of the progressive nature of their learning and future careers. They appeared to clearly distinguish between the ECE and the subsequent learning they will undertake in Phase III of the MBBS, as well as the immediate value of the ECE for their current studies versus its long-term impact on their future clinical practice. This indicates that for the ‘System perspective’ meta-inference, the integration enabled both confirmation and expansion of the overall understanding.
For ‘Patient Centricity’ meta-inference, both the quantitative and qualitative analyses built upon each other. Each method underscored how the ECE acquainted learners with differing people-related aspects, including the importance of developing competencies that enhance patient care. The quantitative ratings reflected learners’ perceptions of distinct elements associated with interpersonal interactions, while the qualitative analysis demonstrated that, in addition to introducing learners to exemplary competencies displayed by healthcare providers, the observational aspect of the ECE helped them acquire a range of interpersonal soft skills. Thus, for the ‘Patient Centricity’ meta-inference, the integration led to both confirmation and expansion of the overall viewpoint.
Concerning the ‘Theory–practice link’ meta-inference, both qualitative and quantitative analyses indicated that the ECE exposed learners to how on-campus learning can be applied in the clinical environment. Moreover, the qualitative analysis revealed that the ability to make clinical correlations varied among learners. In addition to establishing connections related to interpersonal skills, some learners exceeded the intended learning outcomes by noting the pathology of diseases. Consequently, for the ‘Theory–practice link’ meta-inference, the integration once again resulted in both confirmation and expansion of the overall perspective.
In relation to the ‘Resilience’ meta-inference, the quantitative data showed that the learners benefited from the experience. Both the quantitative and qualitative analyses demonstrated that the learners observed competencies and values shared with other healthcare providers, which in turned fostered their professional identity. In addition, the qualitative analysis showed how the ECE further enabled the learners through raising their self-efficacy, motivation, tolerance, and confidence; reinforcing their purpose; identifying role models; exploring interests; and developing foresight. Accordingly, for the ‘Resilience’ meta-inference, the integration again led to both confirmation and expansion of the overall viewpoint.
link